Reproductive health & STIs-
Reproductive health in women encompasses a wide range of physical, emotional, and social well-being related to the reproductive system. It includes not only the absence of diseases or disorders but also the ability to have a satisfying and safe sex life, the capability to reproduce, and the freedom to make choices about one’s reproductive health.
Here are some key aspects of reproductive health in women:
1. Menstrual Health:
– Regular menstrual cycles are a sign of a healthy reproductive system. Irregularities in the menstrual cycle may indicate hormonal imbalances or other health issues.
– Menstrual hygiene is crucial to prevent infections. Proper disposal of menstrual products and maintaining cleanliness are essential.
2. Contraception:
– Access to a variety of contraception methods is essential for women to make informed choices about family planning.
– Contraceptive methods include hormonal birth control, barrier methods, intrauterine devices (IUDs), and permanent sterilization options.
3. Sexually Transmitted Infections (STIs):
Education and awareness about STIs are crucial for preventing their spread. Safe sexual practices, regular testing, and vaccination (e.g., HPV vaccine) are important components of reproductive health.
Sexually Transmitted Infections (STIs), also referred to as sexually transmitted diseases (STDs) or venereal diseases, are infections that are primarily transmitted through sexual activity. They can affect individuals of all ages, genders, and sexual orientations. Here is detailed information on various aspects of STIs:
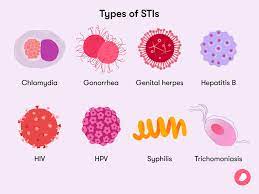
1. Common STIs:
– Chlamydia: Caused by the bacterium Chlamydia trachomatis, it often presents with no symptoms but can lead to serious reproductive health issues if left untreated.
– Gonorrhea: Caused by the bacterium Neisseria gonorrhoeae, it can affect the genital, rectal, and throat areas and may cause symptoms like discharge, pain, and inflammation.
– Syphilis: Caused by the bacterium Treponema pallidum, it progresses through stages and can affect various organs if untreated.
– Human Papillomavirus (HPV): A group of viruses causing genital warts and linked to cervical and other cancers.
– Herpes Simplex Virus (HSV): Causes painful sores, usually around the genital or oral area.
– HIV (Human Immunodeficiency Virus): Attacks the immune system, leading to acquired immunodeficiency syndrome (AIDS).
2. Transmission:
– STIs are primarily transmitted through unprotected sexual activity, including vaginal, anal, and oral sex.
– Some infections can also be transmitted through non-sexual means, such as sharing needles, blood transfusions (rare), or from mother to child during childbirth or breastfeeding.
3. Prevention:
Condom Use: Consistent and correct use of condoms during sexual activity can reduce the risk of STI transmission.
– Vaccination: Vaccines are available for certain STIs, such as HPV. Vaccination can prevent some of the most common and high-risk types of the virus.
– Regular Testing: Routine STI screening is important, especially for individuals with multiple sexual partners or those engaging in high-risk behavior.
– Limiting Sexual Partners: Reducing the number of sexual partners can lower the risk of STI transmission.
4. Symptoms:
– Symptoms vary depending on the specific STI but may include genital sores, pain or burning during urination, unusual discharge, itching, and flu-like symptoms.
– Many STIs, especially in the early stages, may be asymptomatic, emphasizing the importance of regular testing.
5. Diagnosis and Treatment:
– Diagnosis often involves a combination of physical exams, laboratory tests (e.g., blood tests, swabs), and patient history.
– Treatment varies based on the specific STI and may involve antibiotics, antiviral medications, or other prescription drugs.
– Early detection and treatment are crucial to prevent complications and further transmission.
6. Complications:
– Untreated STIs can lead to serious complications, including infertility, pelvic inflammatory disease (PID), certain cancers, and increased susceptibility to HIV.
– Some STIs can also be transmitted from a pregnant woman to her child, leading to congenital infections.
7. Global Impact:
– STIs have a significant global impact on public health, contributing to a range of reproductive and other health issues.
– Efforts to control and prevent STIs include public health campaigns, education, and accessible healthcare services.
8. Stigma and Mental Health:
– Stigma associated with STIs can have negative effects on mental health. Open communication, education, and reducing stigma are important for overall well-being.
9. Partner Notification:
– Individuals diagnosed with an STI should inform their sexual partners so that they can also seek testing and treatment.
It’s important to note that practicing safe sex, getting regular check-ups, and seeking prompt medical attention if symptoms arise are key components of preventing and managing sexually transmitted infections. Open communication with healthcare providers and sexual partners is crucial for maintaining sexual health and well-being.
4. Preconception Care:
Preparing for a healthy pregnancy includes lifestyle factors such as maintaining a balanced diet, exercising regularly, and avoiding harmful substances like alcohol and tobacco.
– Identifying and managing pre-existing medical conditions before conception is crucial for a healthy pregnancy.
5. Pregnancy and Childbirth:
– Prenatal care is essential for monitoring the health of both the mother and the developing fetus during pregnancy.
– Safe and supportive childbirth practices contribute to positive reproductive health outcomes.
6. Postpartum Care:
Physical and emotional well-being after childbirth is vital. Adequate support and care during the postpartum period contribute to a smooth recovery.
Postpartum care refers to the care and support provided to women after childbirth. This period, often referred to as the postpartum or postnatal period, typically spans the first six weeks after giving birth, although it can extend beyond this timeframe. Postpartum care is crucial for the well-being of both the mother and the newborn, addressing physical, emotional, and social aspects of recovery and adjustment. Here are detailed aspects of postpartum care:
1. Physical Recovery:
– Monitoring Vaginal Bleeding: Postpartum bleeding, known as lochia, is normal. However, excessive bleeding or the presence of large clots should be reported to healthcare providers.
– Perineal Care: Proper care of the perineal area, especially if there were tears or an episiotomy during delivery, is essential. Sitz baths, pain management, and keeping the area clean aid in healing.
– Cesarean Section Recovery: For women who underwent a cesarean section, care includes monitoring the incision site, managing pain, and following any specific instructions provided by healthcare professionals.
2. Pelvic Floor Exercises:
– Kegel exercises help strengthen the pelvic floor muscles, promoting bladder and bowel control. These exercises are beneficial for both vaginal and cesarean deliveries.
3. Breastfeeding Support:
– Assistance with breastfeeding techniques and addressing any challenges is crucial during the postpartum period. Lactation consultants and healthcare providers can offer guidance.
– Addressing issues such as nipple pain, engorgement, and establishing a feeding routine.
4. Emotional Well-Being:
Postpartum Depression (PPD) Screening: Regular assessments for postpartum depression and other mood disorders are essential. Early detection allows for prompt intervention and support.
Emotional Support: Emotional well-being is crucial. Mothers may experience a range of emotions, and having a support system in place is vital. This includes partners, family, friends, and healthcare professionals.
5. Nutrition and Hydration:
– A balanced diet with a focus on nourishing foods is important for postpartum recovery, especially if the mother is breastfeeding.
– Adequate hydration is essential, especially if breastfeeding.
6. Rest and Sleep:
– Ensuring that the mother gets sufficient rest is important for recovery. Support from family and friends in managing household tasks allows the mother to focus on self-care and bonding with the newborn.
7. Postpartum Checkups:
– Regular follow-up appointments with healthcare providers are scheduled to monitor the mother’s physical and emotional well-being. Any concerns or complications can be addressed during these visits.
8. Contraception and Family Planning:
– Discussions about contraception options and family planning are often initiated during postpartum care appointments.
9. Resumption of Physical Activity:
– Gradual resumption of physical activity, including exercise, is usually recommended after the postpartum period. However, individual recommendations may vary based on the mother’s health and the type of delivery.
10. Birth Control and Family Planning:
– Discussing and choosing an appropriate method of birth control is often part of postpartum care. This is important for women who wish to space their pregnancies or prevent future pregnancies.
Postpartum care is a comprehensive and individualized process, and the specific details may vary based on factors such as the mother’s health, the type of delivery, and any complications that may have arisen during childbirth. Continuous communication with healthcare providers and access to a supportive network are essential components of effective postpartum care.
7. Infertility:
– Infertility issues can be complex and may involve both male and female factors. Access to fertility treatments, counseling, and support are important aspects of reproductive health.
8. Gynecological Health:
– Regular gynecological check-ups, including pelvic exams and Pap smears, help in early detection and prevention of reproductive health issues, including cervical cancer.
9. Menopause:
– Understanding and managing the physical and emotional changes associated with menopause is crucial for maintaining overall well-being.
10. Counseling and Education:
– Access to information, education, and counseling services on reproductive health empowers women to make informed decisions about their bodies, sexuality, and overall well-being.
Promoting reproductive health involves addressing social, economic, and cultural factors that impact women’s ability to make choices about their reproductive lives. It requires a holistic approach that integrates medical care, education, and support services. Additionally, ensuring access to healthcare services and promoting gender equality are fundamental aspects of advancing reproductive health for women.
World Sexual Health Day(4th september)-
September 4th is recognized as World Sexual Health Day. This day is dedicated to promoting sexual health around the world. While it has a broader focus on sexual health in general, it often includes discussions, events, and initiatives related to preventing and addressing sexually transmitted infections (STIs).
World Sexual Health Day aims to raise awareness about sexual health issues, break down stigma and discrimination, and promote access to accurate information and healthcare services related to sexual well-being.
It’s worth checking with relevant health organizations or international health agencies for any updates or specific activities related to World Sexual Health Day or STI awareness on September 4th, as public health initiatives and awareness days may evolve over time.
For more about vaginal health click here- https://www.womaniyas.com/2024/02/vaginal-microbiota-highlights.html