What Are Fibroids?
Fibroids, also called uterine fibroids or leiomyomas, are non-cancerous growths that develop in or around the uterus.
They are composed of smooth muscle cells and fibrous connective tissue and can vary greatly in size, ranging from very small to large masses that can distort the shape of the uterus.
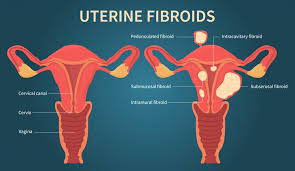
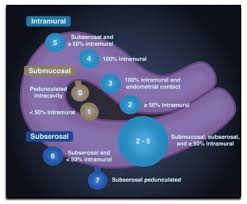
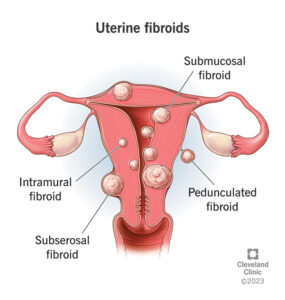
Types –
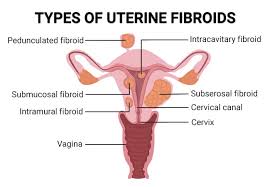
1. Intramural Fibroids: These are the most common type and grow within the muscular wall of the uterus.
2. Subserosal Fibroids: These grow outside the uterus, on its outer surface.
3. Submucosal Fibroids: These grow into the inner cavity of the uterus.
4. Pedunculated Fibroids: These are attached to the uterus by a stalk-like growth, either inside or outside the uterus.
Fibroid- Causes and Risk Factors:
The exact cause of fibroids is not fully understood, but several factors may contribute to their development.
Here are some details about potential causes of it:
1. Hormones:
Estrogen and progesterone, two hormones that regulate the menstrual cycle, are believed to play a significant role in the development and growth of it.
These hormones stimulate the growth of the uterine lining during each menstrual cycle, which may also stimulate the growth of it.
Fibroids tend to grow larger during pregnancy when hormone levels are high, and they usually shrink after menopause when hormone levels decrease.
2.Genetic Predisposition –
There appears to be a genetic component to fibroids, as they often run in families.
Women with a family history of it are more likely to develop them themselves.
Specific genetic mutations or variations may increase the risk of fibroid development.
3. Other Factors:
Several other factors may contribute to the development of fibroids or increase the risk of their occurrence, including:
Race: Fibroids are more common in women of African descent compared to women of other racial/ethnic groups.
Obesity: Being overweight or obese is associated with an increased risk of developing it.
Diet: Some studies suggest that diets high in red meat and low in green vegetables may increase the risk of it.
Vitamin D Deficiency: Low levels of vitamin D have been associated with an increased risk of it.
Environmental Factors: Exposure to certain environmental toxins and chemicals may contribute to the development of it, although more research is needed to understand these relationships fully.
4. Reproductive Factors:
Age at First Menstruation: Women who started menstruating at an early age may have a higher risk of developing it.
Pregnancy: Women who have never been pregnant or have had fewer pregnancies may have a higher risk of developing it.
Hormonal Birth Control: Some studies suggest that the use of hormonal contraceptives such as birth control pills may reduce the risk of fibroids, while others suggest that certain types of hormonal contraceptives may increase the risk.
Overall, fibroids likely develop as a result of complex interactions between genetic, hormonal, and environmental factors.
While these factors may increase the risk of fibroids, they do not guarantee that fibroids will develop, and many women with risk factors never develop them.
Symptoms:
It can cause a variety of symptoms, and the severity and type of symptoms can vary depending on the size, number, and location of the fibroids.
1. Heavy Menstrual Bleeding (Menorrhagia):
One of the most prevalent signs of fibroids is excessive menstrual bleeding.
Women who have fibroids may endure prolonged or heavy menstrual bleeding, necessitating numerous pad or tampon changes. Some people may pass big blood clots during their periods.
2. Menstrual Periods Lasting Longer Than a Week:
It can cause menstrual periods to last longer than usual, sometimes extending beyond a week.
3. Pelvic Pain and Pressure:
It can induce pelvic discomfort or pressure, with varying intensity and duration.
The discomfort might be subtle and achy, or severe and stabbing.
The pressure may feel like heaviness or fullness in the pelvic region.
4. Lower Back Pain:
Fibroids can cause lower back pain, particularly if they press on nerves in the lower back or pelvis.
5. Frequent Urination:
Fibroids that press on the bladder can cause frequent urination or a constant urge to urinate, even when the bladder is not full.
6. Difficulty Emptying the Bladder:
Large fibroids may obstruct the bladder, making it difficult to completely empty the bladder during urination.
7. Constipation: Fibroids that press on the rectum or intestines can lead to constipation or difficulty passing stools.
8. Pain During Intercourse: Fibroids located near the cervix or within the uterus can cause pain or discomfort during sexual intercourse.
9. Enlargement of the Lower Abdomen:
Large fibroids or multiple fibroids can cause the lower abdomen to become enlarged or distended, leading to a noticeable increase in abdominal girth.
10. Infertility or Pregnancy Complications:
Fibroids can sometimes interfere with fertility by obstructing the fallopian tubes or preventing a fertilized egg from implanting.
Fibroids can also raise the possibility of pregnancy issues such as miscarriage, premature delivery, or breech presentation.
It’s crucial to remember that not all women with fibroids will have symptoms.
Some women may have fibroids detected by chance during a pelvic exam or imaging test, and they may not need treatment if they are not having symptoms.
However, for women experiencing symptoms that interfere with their quality of life or reproductive health, treatment options are available to manage fibroids effectively.
Diagnosis:

Fibroids are often diagnosed during a routine pelvic exam or imaging tests, such as ultrasound, MRI, or CT scans.
Fibroids- Treatment Options:
Treatment for fibroids depends on various factors such as the size and location of it, the severity of symptoms, the patient’s age, and their desire for future fertility.
Here are the treatment options for this in detail:
1. Watchful Waiting (Expectant Management):
If these are small, asymptomatic, and not causing any complications, the doctor may recommend a watchful waiting approach.
This involves regular monitoring of symptoms through pelvic exams, ultrasounds, or other imaging tests without active treatment.
2. Medications: Several medications can help manage the symptoms associated with it,
but they do not shrink it themselves.
These medications include:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs such as ibuprofen or naproxen can help alleviate pelvic pain and menstrual cramps associated with it.
Hormonal Birth Control:
Hormonal contraceptives, including birth control pills, patches, or hormonal intrauterine devices (IUDs), can help regulate menstrual bleeding and reduce heavy periods associated with it.
Gonadotropin-Releasing Hormone (GnRH) Agonists:
These drugs briefly induce menopause by reducing estrogen synthesis.
This can shrink it and alleviate symptoms like excessive bleeding and pelvic discomfort.
However, due to possible adverse effects, they are usually used for short-term treatment and are not recommended for long-term usage.
3. Uterine Artery Embolization (UAE):
In this minimally invasive surgery, a radiologist injects microscopic particles into the blood arteries that supply the fibroids, preventing blood flow and causing them to shrink gradually.
UAE is helpful in treating symptoms including excessive menstrual bleeding and pelvic discomfort, and it usually does not need a hospital stay.
4. Myomectomy:
Myomectomy is a surgical procedure to remove fibroids while preserving the uterus.
It may be recommended for women who wish to retain their fertility or avoid a hysterectomy.
Myomectomy can be performed via various techniques, including:
Abdominal Myomectomy: Open surgery through an abdominal incision.
Laparoscopic Myomectomy: Minimally invasive surgery using small incisions and a camera to guide the procedure.
Hysteroscopic Myomectomy: Removal of submucosal fibroids through the cervix using a hysteroscope inserted into the uterus.
5. Hysterectomy:
Hysterectomy involves surgical removal of the uterus and is considered a definitive treatment for fibroids, as it eliminates the possibility of fibroid recurrence.
It may be recommended for women who have severe symptoms, have completed childbearing, or do not wish to preserve their fertility.
6. MRI-guided Focused Ultrasound Surgery (MRgFUS):
MRgFUS is a non-invasive therapy that employs high-intensity focused ultrasound waves to heat and kill fibroid tissue while preserving healthy tissue.
It may be an option for women seeking non-surgical therapy for symptomatic fibroids in particular parts of the uterus.
The choice of therapy is determined by individual circumstances, and it is critical for women to consider the advantages, dangers, and potential consequences of each treatment option with their healthcare professional before making an educated decision.
Conclusion:
Fibroids are common non-cancerous growths in the uterus that can cause a range of symptoms.
Diagnosis and treatment depend on various factors, and women experiencing symptoms should consult with a healthcare provider for proper evaluation and management.
For more women’s related info visit here also – https://womaniyas.com/2024/02/29/premenstrual-syndrome-pms-symptoms-causes-treatment/
