Ulcerative colitis (UC)

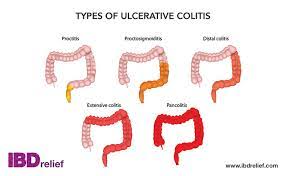
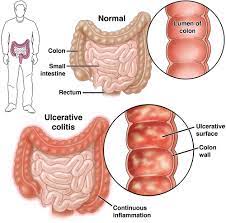
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the colon and rectum. It is characterized by inflammation and ulceration of the inner lining of the colon and rectum, leading to various symptoms including abdominal pain, diarrhea, rectal bleeding, and weight loss. Here are some detailed aspects of ulcerative colitis:
Symptoms:–
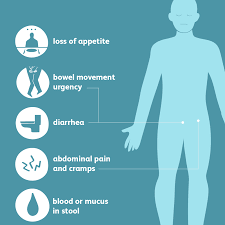
- Diarrhea: Often with blood or pus.
- Abdominal pain and cramping.
- Rectal bleeding: Blood in stool or visible blood on toilet paper.
- Urgency to defecate: The feeling of needing to go to the bathroom urgently.
- Tenesmus: The sensation of needing to pass stool even when the bowel is empty.
- Fatigue.
- Weight loss.
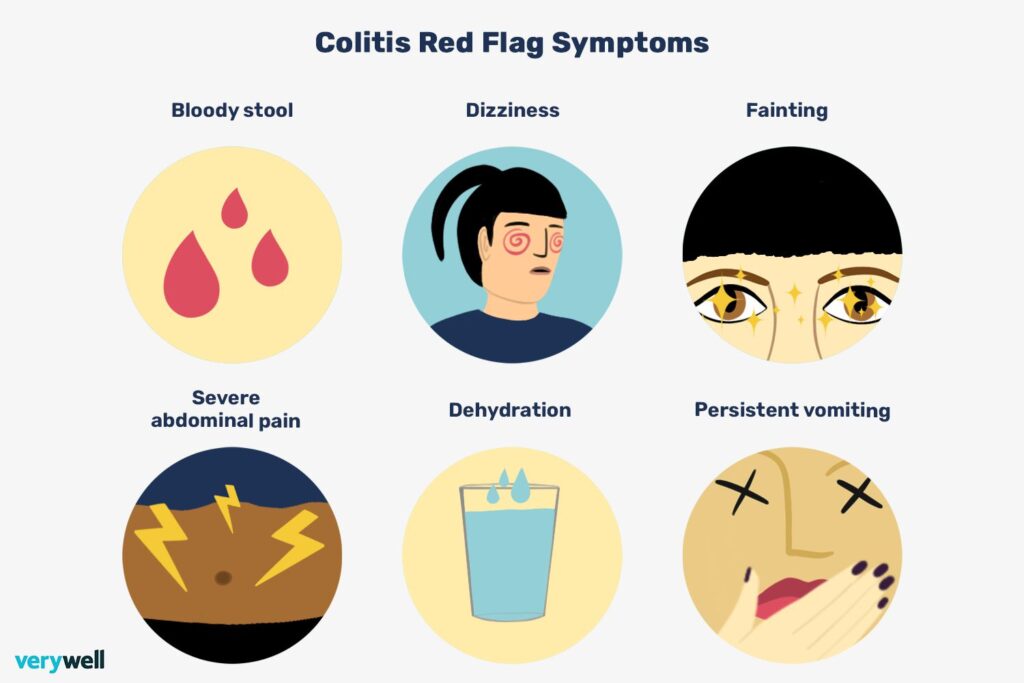
- Fever (in severe cases).
-
Causes:
- The exact cause of ulcerative colitis is unknown, but it’s believed to involve a combination of genetic, environmental, and immunological factors.
- Genetics: There is evidence of a genetic predisposition to UC, with the condition being more common in people with a family history of the disease.
- Immune system: UC is considered an autoimmune disorder, where the immune system mistakenly attacks the lining of the colon and rectum, causing inflammation.
- Environmental factors: Factors such as diet, stress, and exposure to certain bacteria or viruses may trigger or exacerbate UC in susceptible individuals.
-
Diagnosis:
- Medical history and physical examination.
- Blood tests to check for inflammation, anemia, and nutritional deficiencies.
- Stool tests to rule out infections and check for blood in the stool.
- Colonoscopy and sigmoidoscopy: These procedures involve inserting a flexible tube with a camera into the rectum and colon to examine the lining for signs of inflammation, ulceration, or other abnormalities.
- Biopsy: During colonoscopy or sigmoidoscopy, small tissue samples (biopsies) may be taken for examination under a microscope to confirm the diagnosis and rule out other conditions.
-
Treatment:
- Medications: Anti-inflammatory drugs, such as aminosalicylates and corticosteroids, are often prescribed to reduce inflammation and relieve symptoms during flare-ups. Immunosuppressants and biologic therapies may also be used in moderate to severe cases.
- Diet and lifestyle modifications: Certain dietary changes, such as avoiding trigger foods, increasing fiber intake, and staying hydrated, may help manage symptoms. Stress management techniques and regular exercise may also be beneficial.
- Surgery: In cases of severe UC that do not respond to medical treatment or complications such as severe bleeding, perforation of the colon, or increased risk of colon cancer, surgery to remove the colon (colectomy) may be necessary. This procedure can often cure UC but may require a permanent ileostomy or an internal pouch (ileoanal anastomosis) to redirect waste from the body.
-
Complications–
- Severe bleeding.
- Perforation of the colon.
- Toxic megacolon: A life-threatening condition characterized by severe inflammation and dilation of the colon.
- Increased risk of colon cancer, particularly in cases of long-standing and extensive UC.
- Nutritional deficiencies due to malabsorption or loss of nutrients through diarrhea and bleeding.
-
Management:
- Regular monitoring: People with UC often require regular follow-up appointments with gastroenterologists to monitor disease activity, adjust treatment as needed, and screen for complications such as colon cancer.
- Patient education and support: Understanding the condition, its triggers, and how to manage symptoms is essential for improving quality of life and reducing the risk of flare-ups. Support groups and educational resources can provide valuable support and information for patients and their families.
It’s important for individuals with ulcerative colitis to work closely with healthcare providers to develop a personalized treatment plan tailored to their specific needs and disease severity. Early diagnosis and appropriate management can help improve symptoms, reduce inflammation, and minimize the risk of complications associated with UC.
Ulcerative colitis (UC) in women –
Ulcerative colitis (UC) affects both men and women, but there are certain considerations specific to women that are important to address. Here are details regarding ulcerative colitis in women:
-
Prevalence and Onset:
- Ulcerative colitis affects women and men equally in terms of prevalence.
- The onset of UC can occur at any age, but it often peaks between the ages of 15 and 30, and there’s a second peak between the ages of 50 and 70.
- Some studies suggest that women may be more likely to develop UC during their reproductive years, with some evidence indicating that hormonal factors, such as changes in estrogen levels, may influence disease onset and activity.
-
Pregnancy and Fertility:
- Women with ulcerative colitis can have successful pregnancies, but disease activity may influence fertility and pregnancy outcomes.
- Active inflammation and certain medications used to treat UC (such as corticosteroids and immunosuppressants) may affect fertility in women.
- It’s essential for women with UC to discuss family planning and pregnancy with their healthcare providers to optimize disease management and minimize risks during pregnancy.
- Generally, most women with well-controlled UC can have uncomplicated pregnancies, but close monitoring and coordination between gastroenterologists and obstetricians are necessary to ensure the best outcomes for both mother and baby.
-
Menstrual Cycle and Hormonal Factors:
- Some women with UC report changes in disease activity related to their menstrual cycle.
- Hormonal factors, particularly fluctuations in estrogen levels, may influence the course of UC. Some women experience worsening symptoms during certain phases of the menstrual cycle, such as menstruation or ovulation.
- Hormone replacement therapy (HRT) or oral contraceptives may also impact disease activity in some women with UC, although individual responses can vary.
-
Management Considerations:
- Pregnancy planning: Women with UC should discuss family planning with their healthcare providers, as certain medications used to treat UC may need to be adjusted before conception.
- Medication management during pregnancy: Some medications commonly used to treat UC, such as aminosalicylates, are generally considered safe during pregnancy, while others, like corticosteroids and immunosuppressants, may carry more risks and require careful monitoring.
- Menstrual cycle tracking: Keeping track of symptoms throughout the menstrual cycle may help identify patterns and optimize disease management strategies.
- Hormonal therapy: In some cases, hormonal therapy or contraceptives may be used to manage symptoms, regulate menstrual cycles, or control disease activity, although the effectiveness can vary among individuals.
-
Colon Cancer Screening:
- Women with ulcerative colitis, particularly those with long-standing and extensive disease, have an increased risk of developing colon cancer compared to the general population.
- Regular colonoscopies with biopsies are recommended for colon cancer screening and surveillance in individuals with UC, including women.
-
Psychological and Emotional Impact:
- Living with a chronic condition like UC can have a significant psychological and emotional impact on women, including feelings of stress, anxiety, depression, and body image concerns.
- Seeking support from healthcare professionals, support groups, and mental health professionals can be beneficial in addressing these challenges and improving overall well-being.
Overall, managing ulcerative colitis in women involves a holistic approach that considers both disease-specific factors and individual reproductive and hormonal health needs. Open communication with healthcare providers and a personalized treatment plan tailored to each woman’s unique circumstances are essential for optimal disease management and quality of life.
Certainly, here are detailed explanations of the causes, symptoms, and treatment of ulcerative colitis specifically in women:
-
Causes:
- While the exact cause of ulcerative colitis (UC) is unknown, it is believed to involve a combination of genetic, environmental, and immunological factors.
- Genetics: There is evidence of a genetic predisposition to UC, with the condition being more common in individuals with a family history of the disease. This genetic susceptibility may be more pronounced in women.
- Hormonal factors: Hormonal fluctuations, particularly those related to estrogen, may influence the development and course of UC in women. Some studies suggest that hormonal changes during the menstrual cycle, pregnancy, and menopause can affect disease activity.
- Environmental triggers: Factors such as diet, stress, smoking, and exposure to certain infections or environmental toxins may trigger or exacerbate UC in susceptible individuals, including women.
-
Symptoms:
- Women with ulcerative colitis experience symptoms similar to those in men. Common symptoms include:
- Diarrhea: Often with blood or mucus.
- Abdominal pain and cramping.
- Rectal bleeding: Blood in stool or on toilet paper.
- Urgency to defecate.
- Tenesmus: Feeling the need to pass stool even when the bowel is empty.
- Fatigue.
- Weight loss.
- Fever (in severe cases).
- Women may also experience symptoms related to their reproductive health, such as changes in menstrual patterns, pelvic pain, or discomfort during sexual intercourse. These symptoms can sometimes overlap with those of UC, making diagnosis and management more complex.
-
Treatment:
- Medications: The goals of treatment for ulcerative colitis in women are to induce and maintain remission, alleviate symptoms, and reduce inflammation. Commonly prescribed medications include:
- Aminosalicylates: These drugs, such as mesalamine, are often used as first-line treatment to reduce inflammation in the colon.
- Corticosteroids: Oral or rectal corticosteroids may be used to control inflammation during flare-ups.
- Immunomodulators: Drugs like azathioprine, 6-mercaptopurine, or methotrexate may be prescribed to suppress the immune system and maintain remission.
- Biologic therapies: Monoclonal antibodies, such as infliximab, adalimumab, or vedolizumab, target specific molecules involved in the inflammatory process and are used in moderate to severe cases.
- Hormonal therapy: In some cases, hormonal treatments such as oral contraceptives or hormone replacement therapy (HRT) may be used to manage symptoms or regulate menstrual cycles, although their effectiveness in controlling UC symptoms varies among individuals.
- Surgery: Surgery may be necessary for women with severe UC that does not respond to medical therapy or who develop complications such as toxic megacolon, perforation of the colon, or colorectal cancer. Surgical options include removal of the colon (colectomy) with either an ileostomy or ileal pouch-anal anastomosis (IPAA) procedure.
-
Pregnancy and Fertility Considerations:
- Women with UC can have successful pregnancies, but disease activity may influence fertility and pregnancy outcomes.
- It’s important for women with UC to discuss family planning with their healthcare providers, as certain medications may need to be adjusted before conception.
- Generally, most women with well-controlled UC can have uncomplicated pregnancies, but close monitoring and coordination between gastroenterologists and obstetricians are necessary.
- During pregnancy, medications that are safe for both the mother and fetus are preferred, and corticosteroids are generally avoided if possible.
-
Lifestyle Modifications:
- Diet: While diet alone cannot cure UC, certain dietary modifications may help alleviate symptoms and improve overall health. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins, along with adequate hydration, is recommended.
- Stress management: Stress does not cause UC, but it can exacerbate symptoms. Women with UC may benefit from stress-reduction techniques such as relaxation exercises, meditation, yoga, or counseling.
- Regular exercise: Moderate physical activity can help improve overall well-being, reduce stress, and promote gastrointestinal health in women with UC.
In summary, managing ulcerative colitis in women requires a multidisciplinary approach that addresses both gastrointestinal and reproductive health considerations. Treatment plans should be tailored to individual needs, taking into account disease severity, symptoms, reproductive goals, and potential side effects of medications. Open communication between women and their healthcare providers is essential for optimizing treatment outcomes and improving quality of life.
For more info related to women’s health click here – https://womaniyas.com/wp-admin/post.php?post=10&action=edit
