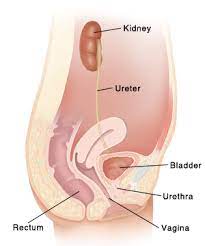
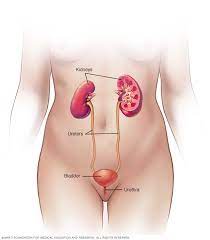
Urinary health in women refers to the condition and function of the urinary tract, which includes the kidneys, ureters, bladder, and urethra. Women are more susceptible to certain urinary tract issues due to anatomical differences, such as having a shorter urethra than men, which can make it easier for bacteria to reach the bladder and cause infections. Here’s a detailed overview of urinary health in women, including common issues and preventive measures:
-
Urinary Tract Infections (UTIs):

- UTIs are bacterial infections that can occur anywhere in the urinary tract but are most commonly found in the bladder (cystitis) or urethra (urethritis).
- Symptoms of UTIs include frequent and urgent need to urinate, burning sensation during urination, cloudy or bloody urine, and pelvic pain.
- Risk factors for UTIs in women include sexual activity, pregnancy, menopause, urinary catheter use, and certain medical conditions that affect the immune system or urinary tract function.
- Treatment typically involves antibiotics prescribed by a healthcare provider based on the type of bacteria causing the infection.
- Urinary Tract Infections (UTIs) are common bacterial infections that can affect any part of the urinary system, including the kidneys, ureters, bladder, and urethra. They occur when bacteria, typically Escherichia coli (E. coli) originating from the gastrointestinal tract, enter the urinary tract and multiply, leading to inflammation and infection. Here’s a detailed overview of UTIs, including causes, symptoms, diagnosis, treatment, and prevention:
-
Causes:
- The most common cause of UTIs is the introduction of bacteria into the urinary tract, often through the urethra. Risk factors for UTIs include:
- Female anatomy: Women have a shorter urethra than men, making it easier for bacteria to reach the bladder.
- Sexual activity: Sexual intercourse can introduce bacteria into the urinary tract.
- Certain birth control methods: Diaphragms and spermicides can increase the risk of UTIs.
- Menopause: Decreased estrogen levels can lead to changes in the urinary tract that increase susceptibility to UTIs.
- Urinary catheter use: Catheters can introduce bacteria directly into the bladder.
-
Symptoms:
- Symptoms of UTIs can vary depending on the location and severity of the infection. Common symptoms include:
- Frequent urination
- Urgent need to urinate
- Burning sensation during urination (dysuria)
- Cloudy or strong-smelling urine
- Blood in the urine (hematuria)
- Pelvic pain or discomfort
- Fever or chills (in more severe cases)
-
Diagnosis:
- A healthcare provider may diagnose a UTI based on a combination of symptoms, medical history, and diagnostic tests such as:
- Urinalysis: Examination of a urine sample for signs of infection, such as bacteria, white blood cells, and red blood cells.
- Urine culture: Laboratory test to identify the specific bacteria causing the infection and determine the most effective antibiotic treatment.
-
Treatment:
- Antibiotics are the primary treatment for UTIs. The choice of antibiotic depends on factors such as the type of bacteria causing the infection and the patient’s medical history. Commonly prescribed antibiotics for UTIs include:
- Nitrofurantoin
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Ciprofloxacin
- Amoxicillin-clavulanate
- It’s essential to complete the full course of antibiotics as prescribed, even if symptoms improve before the medication is finished, to prevent recurrence and antibiotic resistance.
-
Prevention:
- Drink plenty of water to flush bacteria from the urinary tract.
- Urinate promptly after sexual intercourse to help eliminate bacteria.
- Wipe from front to back after using the bathroom to prevent bacteria from entering the urethra.
- Avoid using irritating products such as douches, feminine hygiene sprays, and scented powders.
- Practice good genital hygiene, including washing the genital area with mild soap and water.
- Consider using cranberry products, such as juice or supplements, which may help prevent UTIs by preventing bacteria from adhering to the urinary tract lining. However, evidence supporting the effectiveness of cranberry products is mixed.
- UTIs are typically uncomplicated and respond well to antibiotic treatment. However, recurrent UTIs or complicated UTIs (involving factors such as pregnancy, kidney stones, or underlying medical conditions) may require additional evaluation and management by a healthcare provider. Prompt diagnosis and treatment of UTIs are essential to prevent complications such as kidney infections (pyelonephritis) and recurrent infections.

-
Urinary Incontinence:
- Urinary incontinence refers to the involuntary leakage of urine, which can occur due to weakened pelvic floor muscles, nerve damage, or other factors.
- Types of urinary incontinence in women include stress incontinence (leakage during activities such as coughing, sneezing, or exercise), urge incontinence (sudden, intense urge to urinate followed by leakage), and mixed incontinence (combination of stress and urge incontinence).
- Treatment options may include pelvic floor exercises (Kegels), bladder training, medications, devices such as pessaries, and in severe cases, surgery.
- Urinary incontinence (UI) is a common condition that involves the involuntary loss of urine. It can vary in severity and may have a significant impact on a woman’s quality of life. Here’s a detailed overview of urinary incontinence in women, including types, causes, symptoms, diagnosis, treatment, and prevention:
-
Types of Urinary Incontinence:
- Stress Incontinence: This occurs when pressure on the bladder exceeds the strength of the urethral sphincter, leading to leakage of urine during activities such as coughing, sneezing, laughing, or exercising.
- Urge Incontinence: Also known as overactive bladder, this involves a sudden, intense urge to urinate followed by involuntary leakage of urine. It may be associated with conditions such as bladder irritation, neurological disorders, or muscle dysfunction.
- Mixed Incontinence: This involves a combination of stress and urge incontinence symptoms.
- Overflow Incontinence: This occurs when the bladder doesn’t empty completely, causing it to overflow and leak urine.
- Functional Incontinence: This occurs when physical or cognitive impairments prevent a person from reaching the toilet in time, despite having normal bladder control.
-
Causes:
- Urinary incontinence can result from various factors, including:
- Weakness or damage to the muscles and nerves that control bladder function.
- Hormonal changes, such as those occurring during pregnancy, childbirth, and menopause.
- Pelvic floor disorders, such as pelvic organ prolapse.
- Neurological conditions, such as multiple sclerosis or Parkinson’s disease.
- Certain medications that increase urine production or affect bladder function.
- Chronic conditions that affect mobility or cognition, leading to functional incontinence.
-
Symptoms:
- Symptoms of urinary incontinence may include:
- Involuntary leakage of urine during activities that increase abdominal pressure (stress incontinence).
- Sudden, strong urges to urinate followed by leakage (urge incontinence).
- Frequent urination (frequency).
- Waking up at night to urinate (nocturia).
- Inability to reach the toilet in time due to physical or cognitive impairments (functional incontinence).
-
Diagnosis:
- A healthcare provider may diagnose urinary incontinence based on a combination of medical history, physical examination, and diagnostic tests such as:
- Urinalysis to check for signs of infection or other abnormalities.
- Bladder diary to record fluid intake, urinary frequency, and episodes of incontinence.
- Urodynamic testing to evaluate bladder function and assess urinary flow rates.
- Cystoscopy to examine the inside of the bladder and urethra for any abnormalities.
-
Treatment :
- Treatment options for urinary incontinence may include:
- Behavioral techniques, such as bladder training and scheduled voiding, to improve bladder control.
- Pelvic floor exercises (Kegels) to strengthen the muscles that support the bladder and urethra.
- Medications to relax the bladder muscles (anticholinergics) or increase bladder capacity (beta-3 agonists).
- Vaginal devices, such as pessaries, to support the bladder and reduce leakage.
- Injections of bulking agents into the tissues around the urethra to improve closure and reduce leakage.
- Surgical procedures, such as sling surgery or bladder neck suspension, to support the bladder and urethra.
-
Prevention:
- Maintaining a healthy lifestyle, including regular exercise and maintaining a healthy weight, can help prevent urinary incontinence.
- Practicing pelvic floor exercises (Kegels) can strengthen the muscles that support the bladder and urethra.
- Avoiding irritants such as caffeine, alcohol, and acidic foods and beverages may help reduce urinary symptoms.
- Prompt treatment of conditions such as urinary tract infections and constipation can help prevent exacerbation of urinary incontinence.
- Urinary incontinence is a common and treatable condition, and women should not hesitate to seek medical evaluation and treatment if they experience symptoms of UI. A healthcare provider can provide personalized recommendations based on the type and severity of urinary incontinence, as well as individual preferences and medical history.
-
Pelvic Organ Prolapse:
- Pelvic organ prolapse occurs when the pelvic organs (such as the bladder, uterus, or rectum) descend into the vaginal space due to weakened pelvic floor muscles and ligaments.
- Symptoms may include a feeling of pressure or fullness in the pelvic area, urinary incontinence, difficulty emptying the bladder or bowel, and discomfort during intercourse.
- Treatment options range from conservative measures such as pelvic floor physical therapy and pessaries to surgical repair.
-
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS):
- IC/BPS is a chronic condition characterized by bladder pain, urinary urgency and frequency, and discomfort in the pelvic region.
- The exact cause of IC/BPS is not well understood, but it may involve abnormalities in the bladder lining, nerve dysfunction, or autoimmune factors.
- Treatment may include dietary modifications, bladder training, medications to relieve symptoms (such as pain or inflammation), bladder instillations, and in some cases, surgery.
-
Preventive Measures:
- Stay hydrated by drinking plenty of water.
- Practice good hygiene, including wiping from front to back after using the bathroom.
- Urinate promptly after sexual intercourse to help flush out bacteria.
- Avoid holding urine for prolonged periods.
- Maintain a healthy weight and exercise regularly to support pelvic floor strength.
- Quit smoking, as it can increase the risk of bladder cancer and other urinary tract issues.
- Preventive measures are essential for maintaining women’s health and reducing the risk of various conditions and diseases. Here’s a detailed overview of preventive measures for women:
-
Regular Health Check-ups:
- Schedule regular visits with a healthcare provider for preventive screenings, vaccinations, and health assessments.
- Recommended screenings may include mammograms for breast cancer, Pap smears for cervical cancer, bone density tests for osteoporosis, and blood pressure checks for cardiovascular health.
-
Healthy Diet:
- Eat a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit intake of processed foods, sugary snacks, and foods high in saturated and trans fats.
- Stay hydrated by drinking plenty of water throughout the day.
-
Regular Physical Activity:
- Engage in regular physical activity to maintain a healthy weight, improve cardiovascular health, and reduce the risk of chronic diseases.
- Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, along with muscle-strengthening activities on two or more days per week.
-
Maintain a Healthy Weight:
- Maintain a healthy weight through a combination of healthy eating and regular exercise.
- Aim for a body mass index (BMI) within the healthy range (18.5 to 24.9 kg/m^2).
-
Limit Alcohol and Tobacco Use:
- Limit alcohol consumption to moderate levels (up to one drink per day for women) to reduce the risk of alcohol-related health problems.
- Avoid tobacco use in any form, including smoking and smokeless tobacco, to lower the risk of cancer, cardiovascular disease, and respiratory conditions.
-
Practice Safe Sex:
- Use condoms to reduce the risk of sexually transmitted infections (STIs) and unintended pregnancies.
- Consider regular STI testing, especially if sexually active with multiple partners or engaging in high-risk behaviors.
-
Breast Health:
- Perform regular breast self-exams to check for lumps, changes in breast size or shape, or other abnormalities.
- Schedule regular clinical breast exams and mammograms as recommended by a healthcare provider.
-
Reproductive Health:
- Use contraception consistently and correctly to prevent unintended pregnancies.
- Schedule regular pelvic exams and Pap smears to screen for cervical cancer and other gynecological conditions.
- Discuss reproductive health concerns, family planning, and menopausal symptoms with a healthcare provider.
-
Bone Health:
- Get adequate calcium and vitamin D through diet and supplements if necessary to maintain bone health and reduce the risk of osteoporosis.
- Engage in weight-bearing exercises such as walking, jogging, dancing, or strength training to strengthen bones and muscles.
-
Mental Health
:- Prioritize mental health by managing stress, practicing relaxation techniques, and seeking support from friends, family, or mental health professionals when needed.
- Be aware of signs of mental health conditions such as depression and anxiety and seek help if experiencing symptoms.
-
Regular Eye Exams:
- Schedule regular eye exams to monitor vision health and detect eye conditions such as glaucoma, cataracts, and macular degeneration.
- By adopting these preventive measures and maintaining regular health screenings, women can promote overall well-being and reduce the risk of various health conditions and diseases. It’s essential to work closely with healthcare providers to develop personalized preventive care plans based on individual health needs and risk factors.
Women should consult a healthcare provider if they experience persistent urinary symptoms or changes in urinary habits to receive proper evaluation and management tailored to their individual needs. Regular pelvic exams and screenings can help detect and prevent potential urinary health issues.
For more info about women’s health click here- https://womaniyas.com/2024/02/05/vaginal-microbiota-highlights-the-significance-of-maintaining-a-healthy-microbial-balance-for-overall-reproductive-and-gynecological-healthvaginal-microorganisms-play-a-crucial-role-in-maintaining-the/
