Autoimmune diseases –
Autoimmune diseases are a group of disorders in which the immune system mistakenly attacks and damages the body’s own tissues. The immune system is designed to defend the body against harmful substances like viruses, bacteria, and other pathogens. However, in autoimmune diseases, the immune system fails to recognize certain tissues as “self,” leading to an immune response against normal cells and tissues.
There are many different autoimmune diseases, and they can affect virtually any part of the body. Some common autoimmune diseases include:
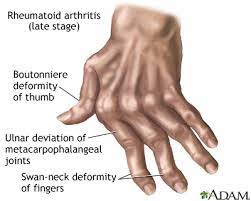
1. Rheumatoid arthritis:
A chronic inflammatory disorder that primarily affects the joints, causing pain, swelling, and stiffness.
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, leading to inflammation, pain, swelling, and eventual joint damage. Unlike osteoarthritis, which is a degenerative joint disease, rheumatoid arthritis involves the immune system attacking the synovium, the lining of the membranes that surround the joints.
Here are key details about rheumatoid arthritis:
1. Symptoms:
Joint pain and swelling: Typically affects small joints, like those in the hands and feet, but can involve larger joints as well.
– Stiffness: Morning stiffness that lasts for more than an hour is a common symptom.
-Fatigue: Many individuals with RA experience persistent fatigue.
– Joint deformities: Over time, RA can lead to joint deformities and loss of function.
2. Causes:
-Autoimmune response: The immune system mistakenly attacks the synovium, triggering inflammation and joint damage.
Genetic Factor – A family history of rheumatoid arthritis may increase the risk.
3. Diagnosis:
– Clinical examination: Evaluation of symptoms, joint involvement, and physical examination.
– Blood tests: Elevated levels of certain antibodies, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP), are often present.
– Imaging: X-rays and other imaging tests can reveal joint damage.
4. Treatment:
–Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologics are commonly prescribed.
– Pain management: Analgesics may be used to relieve pain.
– Physical therapy: Exercises to maintain joint function and mobility.
– Lifestyle changes: Healthy lifestyle choices, such as regular exercise and a balanced diet, can help manage symptoms.
5. Disease Course:
– Variable progression :RA can progress differently in individuals, with periods of flares and remissions.
– Joint damage: Without proper management, RA can lead to joint deformities and disability.
6. Complications:
– Rheumatoid nodules: Firm lumps under the skin.
– Cardiovascular issues: RA is associated with an increased risk of cardiovascular diseases.
– Osteoporosis: Reduced bone density due to inflammation and medication side effects.
7. Management and Prognosis:
–Early intervention: Prompt treatment initiation is crucial to manage symptoms and prevent joint damage.
– Regular monitoring: Follow-up appointments and monitoring of disease activity are important.
– Multidisciplinary approach: Involvement of rheumatologists, physical therapists, and other healthcare professionals.
8. Research and Advances:
– Ongoing research focuses on developing targeted therapies and understanding the underlying mechanisms of RA.
It’s important for individuals with rheumatoid arthritis to work closely with healthcare professionals to create a personalized treatment plan and manage the condition effectively. Early diagnosis and appropriate treatment can significantly improve outcomes and quality of life for individuals with RA.
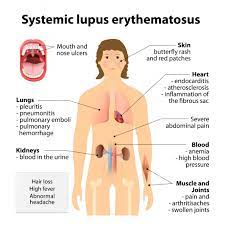
2. Systemic lupus erythematosus (SLE):
A systemic autoimmune disease that can affect various organs, including the skin, joints, kidneys, heart, lungs, and brain.
Systemic Lupus Erythematosus (SLE), commonly referred to as lupus, is a chronic autoimmune disease that can affect various organs and tissues in the body. Here are details about SLE:
1. Symptoms:
Joint pain and swelling: Arthritis is a common symptom, often affecting small joints.
Skin rashes: The characteristic butterfly-shaped rash across the cheeks and nose (malar rash) is a hallmark of lupus.
– Fatigue: Persistent and overwhelming tiredness.
– Fever: Low-grade fevers may occur.
– Photosensitivity: Increased sensitivity to sunlight.
– Organ involvement: SLE can affect the skin, joints, kidneys, heart, lungs, blood cells, and nervous system.
2. Causes:
– Autoimmune response: The immune system attacks the body’s own tissues.
– Genetic factors: A genetic predisposition may contribute, but environmental triggers play a role.
3. Diagnosis:
– Clinical criteria: Physicians often use the American College of Rheumatology criteria for lupus diagnosis.
– Blood tests: Presence of specific antibodies, such as antinuclear antibodies (ANA), anti-double-stranded DNA (anti-dsDNA), and anti-Smith antibodies.
– Other tests: Kidney and liver function tests, complete blood count (CBC), and imaging studies.
4. Treatment:
– Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarial drugs, immunosuppressants, and biologics may be prescribed.
– Lifestyle modifications: Sun protection, regular exercise, and a balanced diet.
5. Disease Course:
– Flares and remissions: Lupus symptoms may vary in intensity over time.
– Chronic condition: SLE is a lifelong condition, but symptoms can often be managed with treatment.
6. Complications:
– Kidney damage: Lupus nephritis is a serious complication affecting the kidneys.
– Cardiovascular issues: Increased risk of heart disease and stroke.
– Lung problems: Inflammation of the lungs may occur.
– Neurological complications: Seizures, headaches, and cognitive issues.
7. Management and Prognosis:
– Individualized treatment: Management is tailored to address specific symptoms and organ involvement.
– Regular monitoring: Ongoing follow-up with healthcare professionals is essential.
– Supportive care: Managing stress and seeking emotional support are important aspects of care.
8. Research and Advances:
– Ongoing research focuses on understanding the underlying causes of lupus and developing targeted therapies.
9. Pregnancy and Lupus:
– Women with lupus can have successful pregnancies but require careful management.
It’s crucial for individuals with SLE to work closely with a rheumatologist or healthcare team to manage symptoms, prevent complications, and improve overall quality of life. Early diagnosis and appropriate treatment are key factors in controlling lupus.
3. Type 1 diabetes:
An autoimmune condition in which the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas.
Type 1 diabetes is a chronic condition characterized by the body’s inability to produce insulin, a hormone that regulates blood sugar (glucose) levels. Unlike type 2 diabetes, which is often associated with lifestyle factors, type 1 diabetes is an autoimmune disease where the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
Here are key details about Type 1 diabetes:
1. Causes:
– Autoimmune Reaction: The exact cause is not fully understood, but it is believed that a combination of genetic and environmental factors triggers an autoimmune reaction where the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas.
2. Onset:
– Usually Early in Life: Type 1 diabetes often develops in childhood or adolescence, but it can occur at any age.
3. Symptoms:
– Polyuria (Excessive Urination): Increased urine production.
– Polydipsia (Excessive Thirst): Feeling extremely thirsty.
– Polyphagia (Excessive Hunger): Experiencing extreme hunger.
– Weight Loss: Unexplained weight loss despite increased appetite.
– Fatigue: Feeling tired and weak.
– Blurry Vision: Changes in vision may occur.
4. Diagnosis:
– Blood Tests: Measurement of blood glucose levels through fasting blood sugar tests, oral glucose tolerance tests, and hemoglobin A1c tests.
– Autoantibody Tests: Detection of autoantibodies associated with the autoimmune destruction of insulin-producing cells.
5. Management:
– insulin Therapy: The primary and essential treatment for type 1 diabetes involves regular insulin injections or the use of an insulin pump.
– Blood Sugar Monitoring: Regular monitoring of blood glucose levels to adjust insulin doses accordingly.
– Meal Planning: Balancing carbohydrate intake with insulin doses, often with the help of a registered dietitian.
– Exercise: Regular physical activity is important but requires careful coordination with insulin and diet.
6. Complications:
– Long-Term Risks: Untreated or poorly controlled type 1 diabetes can lead to serious complications, including cardiovascular disease, kidney damage, nerve damage, and eye problems.
7. Lifestyle Considerations:
– Continuous Care: Type 1 diabetes requires ongoing medical management and regular check-ups.
– Psychosocial Support: Dealing with a chronic condition can have emotional and psychological impacts, so support from healthcare providers, family, and friends is crucial.
8. Research and Advances:
– Ongoing Research: Scientists are continually exploring new treatments, technologies (such as continuous glucose monitoring and artificial pancreas systems), and potential ways to prevent or cure type 1 diabetes.
It’s important for individuals with type 1 diabetes to work closely with healthcare professionals to manage their condition effectively and maintain a healthy lifestyle. Regular monitoring, proper insulin management, and a well-balanced approach to diet and exercise are key components of successful management.
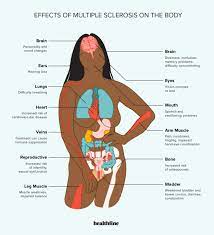
4. Multiple sclerosis (MS):
An autoimmune disease that affects the central nervous system, leading to a range of neurological symptoms.
Multiple Sclerosis (MS) is a chronic autoimmune and neurodegenerative disease that affects the central nervous system (CNS), including the brain and spinal cord. Here are details about MS:
Symptoms –
Fatigue: Persistent and often overwhelming tiredness.
– Muscle weakness: Difficulty with coordination and balance.
– Numbness or tingling: Sensations of pins and needles.
– Vision problems: Blurred vision, double vision, or loss of vision.
– Cognitive issues: Memory problems, difficulty concentrating, and changes in judgment.
– Difficulty walking: Impaired gait and coordination.
– Pain: Chronic pain, often involving muscles or nerves.
– Bladder and bowel dysfunction: Incontinence or constipation.
2. Causes:
–Autoimmune response: The immune system mistakenly attacks the myelin, the protective covering of nerve fibers in the CNS.
– Genetic factors: A family history of MS may increase the risk, but environmental factors also play a role.
3. Types of MS:
Relapsing-Remitting MS (RRMS): Characterized by periods of relapses (exacerbations) followed by partial or complete recovery.
– Secondary-Progressive MS (SPMS): Develops in some individuals with RRMS, characterized by a steady progression of disability.
– Primary-Progressive MS (PPMS): A steady progression of symptoms from the onset without distinct relapses.
4. Diagnosis:
– Clinical criteria: Based on symptoms, medical history, and neurological examination.
– Magnetic Resonance Imaging (MRI): Reveals characteristic lesions in the CNS.
– Cerebrospinal fluid analysis: Presence of certain proteins may support the diagnosis.
5. Treatment:
– Disease-Modifying Therapies (DMTs): Medications to modify the immune response and reduce relapses.
– Symptomatic treatment: Addressing specific symptoms such as pain, fatigue, and muscle spasms.
– Rehabilitation therapies: Physical therapy, occupational therapy, and speech therapy to improve function and quality of life.
6. Disease Course:
– Variable progression: MS progression varies among individuals.
– Fluctuating symptoms: Periods of exacerbations followed by periods of stability or improvement.
7. Complications:
– Mobility issues: Severe cases can lead to mobility impairment and disability.
– Cognitive decline: Some individuals may experience progressive cognitive decline.
– Emotional and psychological impact: Depression and anxiety are common.
8Management and Prognosis:
– Multidisciplinary approach : Involves neurologists, physical therapists, occupational therapists, and other healthcare professionals.
– Regular monitoring: Ongoing assessment of disease activity and response to treatment.
– Supportive care: Addressing emotional and psychological well-being.
9. Research and Advances:
– Ongoing research aims to understand the underlying causes of MS and develop more effective treatments.
Early diagnosis and appropriate management are crucial for individuals with MS to minimize symptoms, prevent relapses, and enhance overall quality of life.
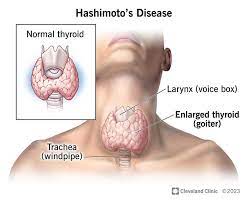
5. Hashimoto’s thyroiditis:
An autoimmune disorder that targets the thyroid gland, causing inflammation and potentially leading to hypothyroidism.
Hashimoto’s thyroiditis, also known as chronic lymphocytic thyroiditis, is an autoimmune disorder that affects the thyroid gland. Here are details about Hashimoto’s thyroiditis:
1. Thyroid Function:
– Thyroid gland: A butterfly-shaped gland located in the neck, producing hormones that regulate metabolism.
2. Symptoms:
– Hypothyroidism: Underactive thyroid function leading to symptoms such as fatigue, weight gain, cold intolerance, and constipation.
– Goiter: Enlargement of the thyroid gland.
– Thyroid nodules: Formation of lumps in the thyroid.
3. Causes:
– Autoimmune response: The immune system mistakenly attacks the thyroid gland, leading to inflammation and damage.
– Genetic factors: A family history of autoimmune diseases may increase the risk.
4. Diagnosis:
– Blood tests: Elevated levels of antibodies, such as anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin antibodies.
– Thyroid function tests: Assess levels of thyroid hormones (T3 and T4) and thyroid-stimulating hormone (TSH).
– Ultrasound: Imaging test to visualize the thyroid gland and detect abnormalities.
5. Treatment:
– Thyroid hormone replacement: Levothyroxine (Synthroid) is commonly prescribed to replace deficient thyroid hormones.
– Monitoring: Regular thyroid function tests to adjust medication dosage as needed.
6. Disease Course:
– Chronic condition: Hashimoto’s thyroiditis is a lifelong condition requiring ongoing management.
– Progression: Over time, the thyroid gland may become less functional, leading to increased dependence on thyroid hormone replacement.
7. Complications:
– Hypothyroidism: The gradual decline in thyroid function can result in a range of symptoms.
– Goiter complications: Large goiters may cause difficulty swallowing or breathing.
– Pregnancy issues: Hashimoto’s can affect fertility and increase the risk of complications during pregnancy.
8. Management and Prognosis:
– Lifelong treatment: Thyroid hormone replacement therapy is usually required.
– Regular monitoring: Periodic blood tests to assess thyroid function.
– Diet and lifestyle: A balanced diet and healthy lifestyle choices can support overall well-being.
9. Research and Advances:
– Ongoing research focuses on understanding the mechanisms of autoimmune thyroid diseases and exploring potential targeted therapies.
Individuals with Hashimoto’s thyroiditis should work closely with an endocrinologist or healthcare professional to manage symptoms effectively and optimize thyroid function. Regular monitoring and adherence to treatment are crucial for maintaining overall health and well-being.
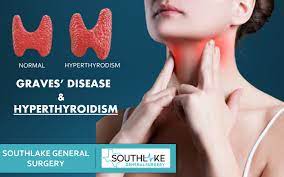
6. Graves’ disease:
An autoimmune condition that affects the thyroid gland, leading to an overproduction of thyroid hormones and hyperthyroidism.
Graves’ disease is an autoimmune disorder that leads to overactivity of the thyroid gland, a condition known as hyperthyroidism. Here are details about Graves’ disease:
1. Thyroid Function:
– Thyroid gland: A butterfly-shaped gland located in the neck, producing hormones that regulate metabolism.
2. Symptoms:
– Hyperthyroidism: Overactive thyroid function leading to symptoms such as weight loss, increased appetite, heat intolerance, nervousness, and rapid heartbeat.
– Goiter: Enlargement of the thyroid gland.
– Graves’ ophthalmopathy: Eye-related symptoms, including bulging eyes (exophthalmos), eye irritation, and double vision.
– Dermopathy: Rarely, thickening and reddening of the skin on the lower legs (pretibial myxedema).
3. Causes:
– Autoimmune response: The immune system produces antibodies (specifically, thyroid-stimulating immunoglobulins or TSI) that stimulate the thyroid gland, leading to increased hormone production.
– Genetic factors: A family history of autoimmune diseases may increase the risk.
4. Diagnosis:
– Blood tests: Elevated levels of thyroid hormones (T3 and T4), low levels of thyroid-stimulating hormone (TSH), and the presence of TSI.
– Radioactive iodine uptake test: Measures the amount of iodine taken up by the thyroid gland.
– Thyroid ultrasound: Imaging test to visualize the thyroid gland and detect abnormalities.
5. Treatment:
– Antithyroid medications: Methimazole and propylthiouracil (PTU) are commonly used to block the production of thyroid hormones.
– Radioactive iodine therapy: Destruction of thyroid cells using radioactive iodine to reduce hormone production.
– Thyroid surgery: Surgical removal of all or part of the thyroid gland (thyroidectomy).
6. Disease Course:
– Variable progression: Graves’ disease can have different courses in individuals, with periods of exacerbation and remission.
– Potential for remission: Some individuals may experience spontaneous remission, while others require ongoing management.
7. Complications:
– Thyroid storm: A rare but severe complication involving a sudden and dangerous increase in thyroid hormone levels.
– Eye complications: Graves’ ophthalmopathy can lead to serious eye issues, including vision loss.
8. Management and Prognosis:
– Lifelong management: Treatment may be required for an extended period, and ongoing monitoring is crucial.
– Thyroid function monitoring: Regular blood tests to assess thyroid hormone levels and adjust treatment as needed.
– Management of eye symptoms: Collaboration with an ophthalmologist for eye-related issues.
9. Research and Advances:
– Ongoing research aims to better understand the underlying causes of Graves’ disease and develop targeted therapies.
Individuals with Graves’ disease should work closely with an endocrinologist or healthcare professional to manage symptoms effectively, prevent complications, and optimize thyroid function. Regular follow-up care and adherence to treatment plans are essential for maintaining overall health and well-being.
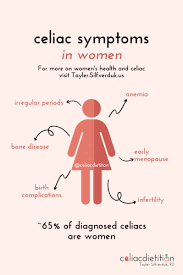
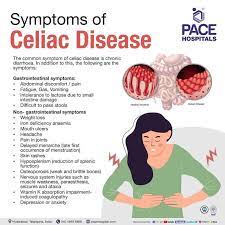
7. Celiac disease:
An autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. It affects the small intestine and can lead to malabsorption of nutrients.
Celiac disease, also known as coeliac disease, is an autoimmune disorder characterized by an abnormal immune response to gluten, a protein found in wheat, barley, rye, and their derivatives. Here are details about celiac disease:
1. Immune Response:
– Autoimmune reaction: In individuals with celiac disease, the immune system responds to gluten by attacking the small intestine, leading to inflammation and damage.
2. Symptoms:
– Gastrointestinal symptoms: Diarrhea, abdominal pain, bloating, and constipation.
– Systemic symptoms: Fatigue, joint pain, headaches, and skin rash.
– Malabsorption: Nutrient deficiencies may lead to weight loss, anemia, and osteoporosis.
3. Genetic Factors:
– Genetic predisposition: Celiac disease has a strong genetic component, and it is more common in individuals with certain genetic markers, especially those carrying the HLA-DQ2 or HLA-DQ8 genes.
4. Diagnosis:
– Blood tests: Detection of specific antibodies, such as anti-tissue transglutaminase (anti-tTG) and anti-endomysial antibodies (EMA).
– Small intestine biopsy: The gold standard for diagnosis involves taking a biopsy of the small intestine to assess damage to the villi.
5. Treatment:
– Gluten-free diet: Complete elimination of gluten-containing foods, including wheat, barley, rye, and their derivatives.
– Nutritional supplements: May be necessary to address nutrient deficiencies.
6. Disease Course:
– Lifelong management: Celiac disease is a chronic condition, and adherence to a gluten-free diet is the primary treatment.
– Resolution of symptoms: Symptoms often improve with a gluten-free diet, and the small intestine may gradually heal.
7. Complications:
– Osteoporosis: Due to calcium and vitamin D malabsorption.
– Infertility: In some cases, celiac disease may contribute to fertility issues.
– Increased risk of other autoimmune diseases: Individuals with celiac disease may have a higher risk of developing other autoimmune conditions.
8. Management and Prognosis:
– Strict gluten-free diet: Requires careful monitoring of food labels and avoiding cross-contamination.
– Regular follow-up: Monitoring for nutritional deficiencies and assessing the effectiveness of the gluten-free diet.
– Education and support: Patients benefit from education about hidden sources of gluten and support from healthcare professionals and support groups.
9. Research and Advances:
– Ongoing research explores new treatments and ways to improve the quality of life for individuals with celiac disease.
It’s crucial for individuals with celiac disease to work closely with healthcare professionals, including dietitians, to ensure proper management, nutritional support, and ongoing monitoring of the condition. Adhering to a strict gluten-free diet is essential for symptom control and preventing complications.
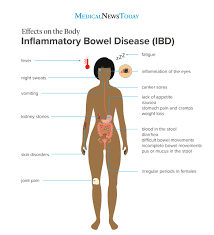
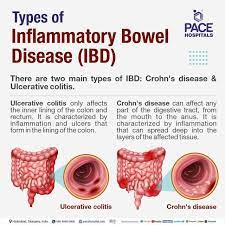
8. Inflammatory bowel disease (IBD):
Including Crohn’s disease and ulcerative colitis, which are chronic inflammatory conditions affecting the gastrointestinal tract.
It seems like you’re asking about Inflammatory Bowel Disease (IBD). IBD is a group of chronic inflammatory conditions of the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis.
1. Crohn’s Disease:
– Location: Can affect any part of the gastrointestinal tract from mouth to anus, but most commonly affects the end of the small intestine (ileum) and the beginning of the colon.
– Characteristics: Inflammation can occur in patches, with normal tissue in between. It can involve all layers of the bowel wall.
– Symptoms: Abdominal pain, diarrhea, weight loss, fatigue, and sometimes symptoms outside the digestive tract like joint pain and skin problems.
2. Ulcerative Colitis:
– Location: Primarily affects the colon and rectum.
– Characteristics: Inflammation typically starts in the rectum and extends continuously along the colon.
– Symptoms: Bloody diarrhea, abdominal cramps, urgency to defecate, and weight loss.
Common Features of IBD:
– Chronic Nature: Both Crohn’s disease and ulcerative colitis are chronic conditions, meaning they persist over time.
– Flare-ups and Remissions: Patients often experience periods of active symptoms (flare-ups) followed by periods of reduced or no symptoms (remissions).
– Unknown Cause: The exact cause of IBD is not known, but it is believed to involve a combination of genetic, environmental, and immune system factors.
– Diagnosis: Diagnosing IBD involves a combination of medical history, physical examination, imaging studies, endoscopy, and laboratory tests.
Treatment:
– Medication: Various medications, including anti-inflammatory drugs, immunosuppressants, and biologics, are used to manage symptoms and control inflammation.
– Dietary Changes: Some individuals find relief from specific dietary changes, and in certain cases, nutritional supplementation may be necessary.
– Surgery: In severe cases or complications, surgery may be required, including removal of a portion of the intestine.
It’s important for individuals with IBD to work closely with healthcare professionals to manage their condition effectively, as the treatment approach may vary based on the severity and specific characteristics of the disease in each person.
The exact causes of autoimmune diseases are not fully understood, but they are thought to involve a combination of genetic and environmental factors. There is currently no cure for most autoimmune diseases, and treatment often focuses on managing symptoms and controlling the immune response. Medications such as corticosteroids, immunosuppressants, and disease-modifying antirheumatic drugs (DMARDs) may be prescribed to help control inflammation and regulate the immune system.
It’s important for individuals with autoimmune diseases to work closely with healthcare professionals to develop a treatment plan that addresses their specific condition and symptoms. Regular monitoring and follow-up care are typically necessary to manage these chronic conditions effectively.